A hemocytometer is a precision glass device that has long been used to count cells using the microscope. The introduction of the hemocytometer marked a significant advancement in the ability to accurately count cells. However, with advancements in technology, the hemocytometer has largely been replaced by automated cell counters. This blog explores what a hemocytometer is, its historical significance, and how automated cell counters have revolutionized cell counting.
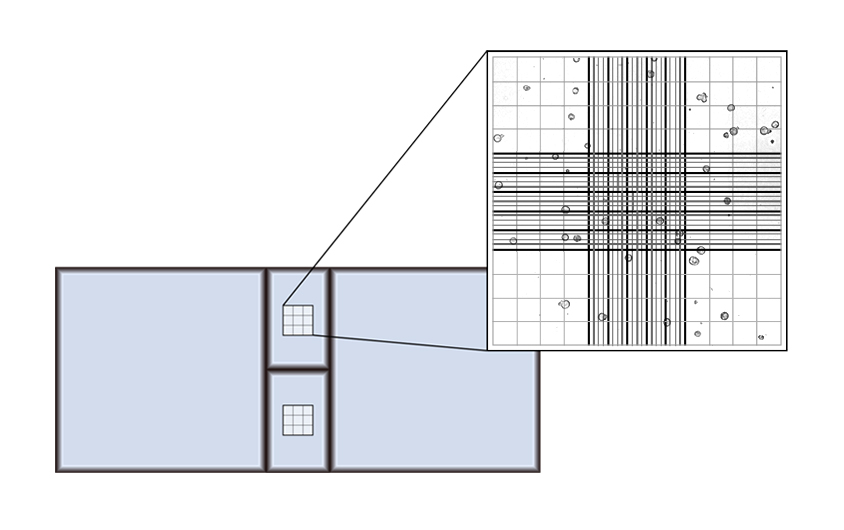
A hemocytometer is a specialized glass device originally designed for counting blood cells. It was invented by French anatomist Louis-Charles Malassez in the late 19th century and has been a staple in laboratories for over a century. The hemocytometer consists of a thick glass microscope slide with a grid etched into the surface. This grid allows scientists to count the number of cells in a specific volume of liquid, enabling them to calculate cell concentration in a sample.
The hemocytometer quickly gained acceptance in scientific laboratories due to its accuracy and ease of use. It became an essential tool for hematologists to count blood cells, for microbiologists to quantify bacterial and yeast cultures, and for cell biologists to measure cell concentrations in various types of suspensions. Over time, the hemocytometer’s design was standardized, with improvements in the precision of the etched grid and the manufacturing of the glass chambers.
As the hemocytometer’s use spread, several enhancements and variations were developed to suit specific applications:
Improved Grid Patterns: Various grid patterns were introduced to accommodate different cell types and concentrations, such as the Neubauer, Improved Neubauer, and Burker grids.
Dual-Chamber Designs: Hemocytometers with dual chambers allowed for simultaneous counting of duplicate samples, increasing reliability and accuracy.
Materials and Manufacturing: Advances in glass manufacturing techniques improved the durability and precision of hemocytometers, making them more robust and easier to use.
Preparation: A cell suspension is mixed with a dye, such as Trypan blue, to distinguish live cells from dead ones.
Sample Loading: A small volume of this mixture is placed on the hemocytometer’s grid.
Cell Counting: Using a microscope, cells within the grid are counted manually. Typically, the number of cells in several squares is averaged to improve accuracy.
Calculation: The concentration of cells in the original suspension is calculated based on the counted cells and the volume of fluid.
The hemocytometer was a breakthrough in cell counting technology. Before its invention, estimating cell concentration was a laborious and imprecise process. The hemocytometer allowed for more accurate and reproducible cell counts, significantly advancing research in fields such as hematology, microbiology, and cell biology. Its relatively simple design and ease of use made it accessible to laboratories worldwide.
Despite its widespread use, the hemocytometer has several limitations:
Time-Consuming: Manual counting is labor-intensive and time-consuming, especially for large numbers of samples.
Subjectivity: Human error and variability can affect the accuracy and reproducibility of the results.
Labor-intensive: Counting cells manually can be tedious, leading to fatigue and decreased precision over time.
Throughput: Accurate counts require skilled technicians, which can limit throughput and efficiency.
In recent decades, automated cell counters have emerged as a superior alternative to hemocytometers. These devices leverage advanced technologies such as image analysis, flow cytometry, and electrical impedance to count cells rapidly and accurately.
Automated cell counters offer numerous benefits over traditional hemocytometers:
Speed: Automated systems can process and count cells in a fraction of the time required for manual counting.
Accuracy: Software algorithms and consistent methodology reduce human error and increase accuracy.
Reproducibility: Automated systems provide more consistent results by eliminating human error and subjectivity.
Ease of Use: Minimal training is required, allowing for greater accessibility and efficiency in the laboratory.
Data Richness: Many automated counters offer additional data outputs, such as cell viability, size distribution, and cell cluster information, providing deeper insights into samples.
The hemocytometer has served as a cornerstone of cell counting in laboratories for over a century. However, the advent of automated cell counters has transformed this essential task, offering unparalleled speed, accuracy, and convenience. As technology continues to advance, automated cell counters will likely become even more integral to research and clinical applications, driving further discoveries and innovations in the life sciences.
In conclusion, while the hemocytometer remains a valuable educational tool and a testament to the ingenuity of early scientific instrumentation, automated cell counters have undeniably taken the lead in modern cell counting, increasing efficiency and precision in laboratory practice.